Lee A. Tan1, Jin Ye Yeo2
1Department of Neurosurgery, UCSF Medical Center, San Francisco, USA; 2JSS Editorial Office, AME Publishing Company
Correspondence to: Jin Ye Yeo. JSS Editorial Office, AME Publishing Company. Email: jss@amegroups.com
This interview can be cited as: Tan LA, Yeo JY. Meeting the Editorial Board Member of JSS: Dr. Lee A. Tan. J Spine Surg. 2024. Available from: https://jss.amegroups.org/post/view/meeting-the-editorial-board-member-of-jss-dr-lee-a-tan.
Expert introduction
Dr. Lee A. Tan (Figure 1) is an assistant professor in the Department of Neurosurgery at UCSF Medical Center in San Francisco, California, USA. He specializes in both minimally invasive and traditional open-surgical techniques for the treatment of various spinal disorders. His clinical focus includes spinal deformities (scoliosis, kyphosis, “flat-back” syndrome, “chin-on-chest” deformity), cervical spine pathologies (cervical disc herniation, cervical stenosis, OPLL), and degenerative lumbar spine pathologies (disc herniation, spinal stenosis, spondylolisthesis). He also has expertise in robotic spine surgery, as well as motion-preservation techniques such as cervical artificial disc replacement and cervical laminoplasty, which can lead to superior clinical outcomes in well-selected patients. Another unique aspect of Dr. Tan’s training is that he received both neurosurgical and orthopedic spine surgery training, which enables him to assess spinal pathologies from an interdisciplinary perspective to select the most appropriate treatment tailored to each patient. Dr. Tan’s research interests include spinal deformity outcome, motion preservation techniques, robotic spine surgery, minimally invasive techniques, and spinal cord injury.

Figure 1 Dr. Lee A. Tan
Interview
JSS: What initially drew you to specialize in spinal deformities and spinal surgery?
Dr. Tan: Initially, my plan was to become a cerebrovascular neurosurgeon. However, during my third year of residency, I experienced a transformative moment on a trauma rotation where I encountered numerous cases of spinal trauma. The intricate biomechanics of the spine and the complexity of surgical decision-making deeply fascinated me. With my undergraduate engineering background, I found that spine surgery perfectly combined technical precision with creative problem-solving, and I felt an undeniable passion for the field.
I am profoundly grateful to have been guided by world-class mentors such as Drs. Vince Traynelis, Richard Fessler, Dan Riew, and Dr. Larry Lenke. Their wisdom, experience, and mentorship have been invaluable in shaping my career. They inspired me to strive for excellence, avoid potential complications, and develop a deeper understanding of the art and science of spine surgery. In gratitude for the mentorship and opportunities I have received, I am deeply committed to fostering the next generation of surgeons by teaching medical students, residents, and fellows. Through education, research, and innovation, I aim to advance the field while continually improving care for my patients. By sharing my knowledge and experiences, I hope to contribute meaningfully to the growth of the profession and honor the legacy of those who guided me.
JSS: Can you share the journey of incorporating robotic spine surgery into your practice? What challenges did you face along the way, and how did you overcome them?
Dr. Tan: My introduction to robotic spine surgery came during my residency training more than a decade ago, where I had the opportunity to work with early robotic systems and witness firsthand the potential they held for enhancing precision and improving outcomes. Over time, I became increasingly involved in implementing robotics into my practice, and I performed the first robotic spine surgery case using the Mazor X Stealth Edition at UCSF many years ago.
Incorporating robotics was not without its challenges. One of the most frequently cited hurdles in the adoption of robotics is the extended setup time compared to traditional navigation systems. To overcome this, building a highly skilled and cohesive surgical team is very important. This will include refining our workflows, rehearsing setups, and leveraging team coordination to significantly reduce setup times and streamline the integration of robotics into routine practice.
Another common challenge is the learning curve associated with adopting new technology. By investing time in simulation training, cadaver labs, and close collaboration with experienced peers, one can shorten the learning curve and reduce complications during the early phase of adaptation.
Additionally, the high costs of robotic systems remain a barrier for many institutions. Addressing this requires creativity and collaboration. By working closely with industry partners, we explored innovative financing models and resource-sharing solutions to make robotics more accessible. These partnerships not only facilitated adoption but also ensured that we could offer the best possible care to our patients.
Looking forward, I am optimistic about the future of robotics in spine surgery. As the technology evolves to include capabilities beyond screw placement, it will further enhance its value in treating a broader range of spinal conditions.
JSS: What are some of the most promising developments in motion-preservation techniques like cervical artificial disc replacement and laminoplasty? How do you foresee these techniques impacting the future of spine surgery?
Dr. Tan: The spine is a remarkable structure that provides both stability and mobility and preserving its natural biomechanics is a cornerstone of modern spine surgery. While fusion remains an essential tool for addressing many spinal pathologies, its inherent drawbacks—such as altering natural spinal mechanics and the potential for adjacent segment degeneration—have driven innovation in motion-preservation techniques.
Cervical artificial disc replacement has emerged as a highly promising option, offering patients relief from degenerative conditions while maintaining motion at the treated segment. Similarly, laminoplasty has provided an effective alternative to laminectomy with fusion, particularly for patients with multilevel cervical stenosis. These techniques minimize disruption to the natural function of the spine and reduce long-term complications associated with adjacent segment disease.
Looking ahead, advancements in lumbar facet joint replacement and other emerging technologies are particularly exciting. These innovations open new avenues for treating pathology while preserving motion and spinal alignment. For instance, advancements in materials science have improved the durability and performance of implants, while enhanced imaging and navigation technologies ensure precise placement and better patient outcomes.
It is important to acknowledge that the successful application of motion-preservation techniques hinges on careful patient selection. Not all patients are candidates for these procedures, and understanding their unique pathology, biomechanics, and overall health is critical to achieving optimal results. For cases where motion preservation is not suitable, fusion will continue to be a reliable and effective approach, particularly in trauma, deformity correction, and severe degenerative conditions.
The future of motion preservation is bright, with ongoing research and technological improvements promising to expand the range of treatable conditions. As surgeons, our responsibility is to integrate these innovations thoughtfully, ensuring that we continue to prioritize patient-centered care and long-term outcomes.
JSS: With your expertise in both traditional and advanced techniques, how do you determine the best surgical approach for your patients? Can you share a case where a novel approach significantly improved a patient's outcome?
Dr. Tan: Choosing the optimal surgical approach is a highly individualized process guided by a few overarching principles. First, it is critical to identify the root cause of the patient’s symptoms. This involves determining whether the primary issue stems from neural compression, instability, spinal malalignment, or a combination of these factors. Once the underlying pathology is understood, I assess whether a motion-preserving technique can effectively address the issue while minimizing long-term biomechanical disruption. My goal is always to choose the least invasive yet most effective approach that aligns with the patient’s unique anatomy, pathology, and overall health.
Patient factors also play a central role in decision-making. For instance, a young, active individual with mild spinal instability may benefit from a motion-preserving technique, such as an artificial disc replacement. In contrast, an elderly patient with significant deformity and osteoporosis may require a more robust fusion-based approach. Additionally, I consider the patient’s overall health and ability to tolerate a more invasive procedure, tailoring my recommendations to balance surgical efficacy with safety and recovery.
One case that stands out involved a patient with severe cervical kyphosis and ossification of the posterior longitudinal ligament (OPLL), resulting in multi-level ventral spinal cord compression. Traditionally, such cases are managed with a multi-level corpectomy, which carries significant risks, including ventral cerebrospinal fluid (CSF) leaks and postoperative instability. Instead, I opted for a novel technique known as vertebral body sliding osteotomy (VBSO). This approach allowed me to decompress the spinal cord effectively without the need for extensive bone removal (Figure 2). By maintaining the structural integrity of the vertebral bodies, I minimized the risk of complications and provided a more stable postoperative outcome.
I first learned this technique during an international visit with Dr. Dong-ho Lee in Korea, underscoring the importance of global collaboration and the exchange of ideas. The patient’s recovery was remarkable, with significant improvement in neurological function and a rapid return to daily activities.
This case exemplifies how blending traditional techniques with innovative approaches can significantly enhance patient outcomes. As surgeons, we must remain open to learning and adopting new methods while grounding our decisions in the principles of safety, efficacy, and patient-centered care. Continuous education, research, and collaboration are essential to refining our practice and offering patients the best possible solutions.
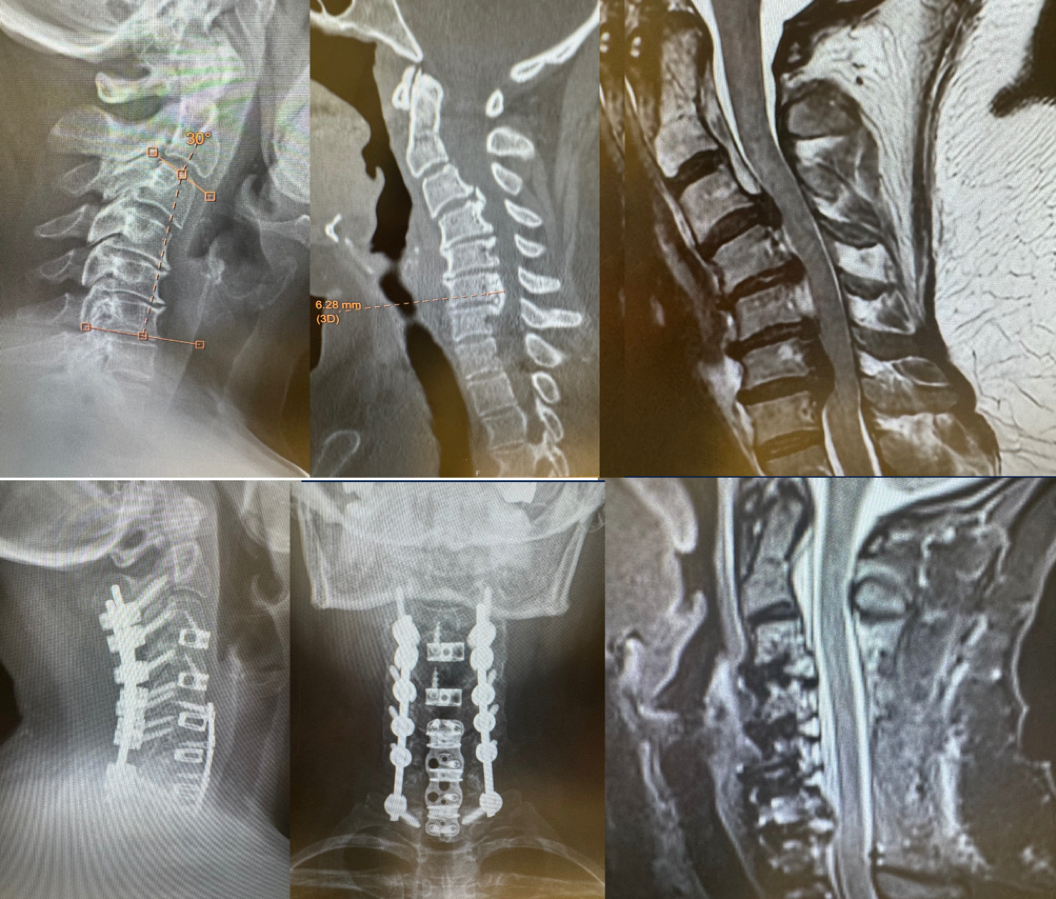
Figure 2 Vertebral body sliding osteotomy (VBSO)
JSS: Where do you see the field of minimally invasive spinal surgery heading in the next decade? Are there any emerging technologies or techniques that you are particularly excited about?
Dr. Tan: Minimally invasive spine surgery (MISS) has transformed the field by reducing the surgical footprint, decreasing recovery times, and improving outcomes for patients. Over the next decade, I anticipate that MISS will continue to evolve, driven by advancements in technology, materials, and surgical techniques.
One area of significant growth is endoscopic spine surgery. These techniques allow for precise treatment of conditions such as lumbar stenosis, foraminal stenosis, far-lateral and thoracic disc herniations, all through small incisions. The development of high-definition optics, better irrigation systems, and improved instrumentation have enhanced the safety and efficacy of these procedures, making them more accessible to surgeons worldwide. In the future, expanded applications of endoscopic surgery will likely include more complex pathologies, such as deformities and multi-level stenosis.
Robotics is another area poised to revolutionize MISS. Current robotic systems have been highly effective in improving accuracy in screw placement and reducing radiation exposure for surgeons and staff. However, the future holds even greater promise as robotics expand to include capabilities like soft tissue manipulation, interbody placement, and integration with AI-driven planning software. These advancements could enable real-time intraoperative adjustments and predictive analytics to optimize surgical outcomes.
Artificial intelligence (AI) and machine learning will play a key role in the future of spine surgery. AI has the potential to analyze large datasets to improve preoperative planning, predict patient-specific risks, and guide surgical decision-making. For instance, AI algorithms can identify patterns in imaging and clinical data that may not be immediately apparent to the human eye, aiding in more precise diagnoses and tailored treatment plans. Additionally, machine learning could enhance robotic capabilities, creating a synergistic relationship between surgeon expertise and technological precision.
Looking ahead, the integration of these innovations will fundamentally reshape the landscape of spine surgery. MISS will continue to push the boundaries of what is possible, offering patients less invasive options with quicker recoveries and better long-term outcomes. As surgeons, our role is to embrace these advancements thoughtfully, ensuring that they are applied in ways that prioritize safety, efficacy, and patient-centered care.
JSS: What advice would you offer to medical students or residents interested in pursuing a career in spine surgery?
Dr. Tan: Spine surgery is an incredibly rewarding and dynamic field, offering a unique blend of intellectual challenge, technical precision, and profound impact on patients’ lives. My first piece of advice is to understand and appreciate the intrinsic rewards of this specialty. There is nothing quite like the gratification of seeing a patient recover and regain their quality of life because of something you did. Whether it’s relieving debilitating nerve pain, correcting a deformity, or restoring mobility, the results of your work are often immediate and life-changing for the patient.
Moreover, the field of spine surgery is continuously evolving, with immense room for innovation. Advancements in robotics, artificial intelligence, motion-preservation techniques, and biologics are just the tip of the iceberg. As a spine surgeon, you have the opportunity to be at the forefront of this transformation, contributing to advancements that could shape the future of medicine. For those who are curious, creative, and driven, spine surgery offers endless possibilities for innovation and growth.
One of the most fulfilling aspects of this career is the balance it provides between science and artistry. Each case presents a unique puzzle, requiring you to apply anatomical knowledge, surgical skills, and critical thinking to develop the best solution for your patient. If you enjoy challenges and the satisfaction of solving complex problems, this field will be deeply fulfilling.
It is also important to highlight that if you truly love what you do, it never feels like work. The passion you bring to this field will sustain you through the long hours, the rigorous training, and the challenges that come with being a surgeon. As the saying goes, “If you love what you do, you’ll never work a day in your life.” For me, the privilege of helping patients, innovating, and teaching others in this field makes every day exciting and rewarding.
For medical students and residents considering this path, I encourage you to seek out strong mentorship. Having a mentor who can guide you through the complexities of this specialty is invaluable. Take the time to immerse yourself in the operating room, engage in research, and attend conferences to gain a broader perspective of the field. Explore the different subspecialties within spine surgery to find what resonates with you most.
Finally, remember that while spine surgery is a demanding field, it is also immensely gratifying. The hard work, dedication, and sacrifices required during training are well worth it when you witness the transformative impact of your efforts on your patients’ lives. If you’re passionate about making a difference, solving complex problems, and continuously learning, spine surgery offers an unparalleled career.
JSS: How has your experience been as an Editorial Board Member of JSS?
Dr. Tan: Serving as an Editorial Board Member of JSS has been a tremendous privilege and a deeply rewarding experience. JSS has established itself as an indispensable resource for spine surgeons worldwide, offering high-quality research, critical reviews, and thought-provoking special issues that address some of the most pressing and relevant topics in our field. Personally, it has been immensely gratifying to be part of this process, whether it is reviewing manuscripts, contributing to special issues, or engaging with the global spine surgery community through the journal. I also want to take this opportunity to recognize and sincerely thank the JSS editorial staff for their exceptional dedication and hard work. The progress and influence JSS enjoys today are a direct result of their tireless efforts and passion for advancing the field of spine surgery. It has been an honor to collaborate with such an extraordinary team.
JSS: As an Editorial Board Member, what are your expectations for JSS?
Dr. Tan: My vision for JSS is one of continued growth and excellence. The journal has already achieved remarkable success, and I firmly believe it is poised to make an even greater impact on the field of spine surgery. I anticipate that JSS will further expand its influence by embracing diverse perspectives, fostering global collaboration, and continuing to prioritize the dissemination of high-quality, evidence-based research.
Personally, I remain committed to supporting JSS in every way I can. Whether through contributing to editorial initiatives, or promoting innovative research, I look forward to working closely with the JSS team to ensure the journal continues to thrive. Together, with the dedicated editorial staff and visionary leadership, I am confident that JSS will continue to set new benchmarks for excellence.
