
Limited morbidity and possible radiographic benefit of C2 vs. subaxial cervical upper-most instrumented vertebrae
Introduction
Cervical deformity (CD) is a complex pathology associated with a wide range of etiologies and presentations, commonly manifesting in cervical kyphosis. Given the heterogenous nature of CD, a wide range of surgical techniques exist for operative management of CD, including anterior-only, posterior-only, and combined surgical approaches. Regardless of the case-specific surgical options, the primary goals of CD-corrective surgery are unchanging: improvement of health-related quality of life (HRQL), creation of a biomechanically secure fusion construct, achievement of solid bony fusion, and restoration of harmonious cervical alignment (1).
Fixation at the second cervical vertebra (C2) has been shown to provide substantial segmental control and 3 column stability in both cadaveric studies and clinical studies in surgical spine populations (2,3). Although patient-specific anatomy, deformity location, deformity flexibility, and degeneration of adjacent levels are all important considerations in the surgical planning process, C2 is typically considered an effective anchoring location for posterior instrumentation, particularly pedicle screws, due to its relatively large pedicle diameter as compared to subaxial vertebrae (4,5). In contrast, fixation in the subaxial cervical spine, while routinely performed for cervical instability, is considered to be more precarious due to risk of laminar cortical breach, facet joint violation, and neurovascular anatomy from C3−C6 (6). For older patients and patients with poor bone quality who are indicated for subaxial fixation, extension of the fusion to C2 may provide a stronger instrumentation construct; however, this is underexplored in the literature.
To date, the literature is lacking studies demonstrating clinical and radiographic indications for extending CD-corrective fusions from the subaxial spine to C2. As such, the purpose of this study was to assess differences in both radiographic alignment and clinical outcomes between surgical CD patients with subaxial upper-most instrumented vertebrae (UIV) and patients with UIV at C2. We hypothesize that amongst severe cervical deformities, CD-corrective fusions with instrumentation ending at C2 allow for optimal fixation and restoration of alignment, while achieving equivocal operative outcomes, equivocal loss of function, and limited patient morbidity.
Methods
Data source
This study is a retrospective review of a prospective, multicenter CD database. Consenting patients were consecutively enrolled at 13 surgical centers across the United States from 2013−2017. All participating centers obtained Institutional Review Board approval prior to patient enrollment. Inclusion criteria for the database were age >18 years and radiographic evidence of CD, as defined by the presence of at least one of the following on baseline imaging: cervical kyphosis (C2−C7 sagittal Cobb angle >10°), cervical scoliosis (C2−C7 coronal Cobb angle >10°), C2−C7 sagittal vertical axis (cSVA) >40 mm or chin-brow vertical angle (CBVA) >25°. Additional inclusion criteria for the present analysis included available 1-year postoperative (1Y) sagittal radiographic imaging and UIV at or cranial to C2.
Data collection and radiographic assessment
Standardized data collection forms captured patient demographics, comorbidities, and imaging studies at the preoperative interval. Operative and complication data were collected following surgery. Standardized HRQL measures were administered at baseline and 1Y study intervals, and included the neck disability index (NDI), numeric rating scale (NRS) for both neck and back pain, the modified Japanese Orthopedics Association (mJOA) outcomes questionnaire, and the EuroQol 5-dimensions 3-severity-level (EQ-5D) questionnaire.
Preoperative standing lateral radiographs were collected at baseline and 1Y intervals, and analyzed with SpineView® (ENSAM, Laboratory of Biomechanics, Paris, France) software as previously published (7-9). Cervical spine flexibility was assessed at 1Y using cervical lateral flexion and extension radiographs. Global sagittal alignment was assessed based on the sagittal vertical axis (SVA, C7 plumbline relative to the posterosuperior corner of S1). Regional radiographic parameters, including thoracic kyphosis (TK; T4−T12), lumbar lordosis (LL; L1−S1), pelvic tilt (PT), pelvic incidence (PI), T1 slope, C2−C7 SVA, cervical lordosis (CL), C0−C2 lordosis, and McGregor’s Slope (McGS), were measured as previously described in the literature (10-12). Mismatch between PI and LL (PI-LL) and the cervical analogue, mismatch between T1 slope and CL (TS-CL), were calculated as assessments of harmonious lumbopelvic and cervical alignment, respectively.
Statistical analysis
Patients were grouped by UIV: C2 or subaxial (C3−C7). To control for differences in preoperative cervical sagittal alignment, the two groups were propensity score matched (PSM) for cSVA. Propensity score matching is a regression-based case control matching technique that simulates a randomization process, effectively attenuating differences between groups in measured independent variables (13). Demographic, radiographic, clinical, and surgical variables were summarized using means and standard deviations for continuous variables, and frequencies and percentages for categorical variables. Differences in baseline demographics, surgical factors, radiographic alignment, and clinical outcomes between groups were assessed using independent samples independent samples t-tests for normally distributed continuous variables, Mann Whitney U tests for non-normally distributed continuous variables, chi-squared tests for categorical variables, and Fisher exact tests for categorical comparisons with expected counts less than 5. Baseline to 1Y changes in alignment were assessed with paired samples t-tests for normally distributed parameters, and Wilcoxon signed-rank tests for non-normal parameters.
All statistical analysis was performed using SPSS software (v23.0, IBM, Armonk, NY, USA).
Results
Patient and surgical overview
This study included 84 patients (63% female, 61±11 years, 29.4±8.3 kg/m2) undergoing surgical management for CD (7.6±3.5 levels fused, 33.3% posterior-only approach, 17.9% anterior-only, 48.8% combined). Overall, there were 43 patients with a C2 UIV and 41 patients with a subaxial UIV. UIV groups did not differ in age (P=0.059), sex (P=0.157), BMI (P=0.922), or Charlson comorbidity index score (P=0.222); however, C2 UIV patients underwent longer fusions (subaxial UIV: 6.0 levels vs. C2 UIV: 9.0, P<0.001) and presented with more severe baseline radiographic deformity, including cSVA (subaxial UIV: 38 mm vs. C2 UIV: 41 mm), C2 slope (subaxial UIV: 45° vs. C2 UIV: 35°), and McGS (subaxial UIV: 8.7° vs. C2 UIV: 1.5°). After propensity score matching, 62 patients were included: 31 subaxial UIV, and 31 C2 UIV. Primary apex of CD did not differ between UIV groups (P=0.464). Differences between C2 UIV and subaxial UIV patients with respect to demographics, comorbidity burden, and surgical factors are outlined in Table 1.
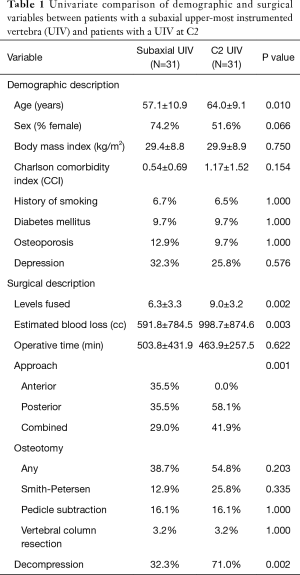
Full table
Overall alignment outcomes
In the overall matched cohort, surgery effectively addressed cervical and upper-cervical malalignment, with the overall cohort showing significant baseline to 1Y improvements in TS-CL (40.4° to 28.1°, P<0.001), cSVA (40.2 mm to 34.5, P=0.005), C0−C2 lordosis (34.5° to 29.2°, P=0.005), and McGS (5.7° to −1.1°, P=0.004). These changes were accompanied with significant improvement in global alignment, as assessed by SVA (4.5 to 26.5 mm, P=0.003). There were no baseline to 1Y changes in spinopelvic alignment, as assessed by PT (18.5° to 18.1°, P=0.602) and PI-LL (0.1° to 1.1°, P=0.407); however, the overall cohort showed a significant baseline to 1Y increase in TK (40° to 44°, P=0.003) and T1 slope (30.5° to 35.1°, P=0.003).
Alignment outcomes by UIV group
Prior to surgery, C2 UIV patients presented with significantly greater McGregor’s Slope than subaxial UIV patients (subaxial UIV: 0.7° vs. C2 UIV: 10.4°, P=0.022), indicating greater disruption of horizontal gaze. All other cervical, thoracic, and global parameters did not differ between groups at baseline: TS-CL, cSVA, C0-C2, C0, C1, C2, and T1 slopes, TK, SVA, PT, and PI-LL (all P>0.050). Similarly, baseline to 1-year postoperative changes in radiographic alignment did not differ between groups for any of the aforementioned radiographic parameters (all P>0.050). Table 2 summarizes baseline to 1-year postoperative changes in alignment within UIV groups. Of note, while both subaxial and C2 UIV patients improved in CL and McGregor’s slope by 1Y (Table 2), C2 UIV patients improved in both of these parameters to a greater degree (for CL, subaxial UIV: 15.9° vs. C2 UIV: 18.4°; for McGS, subaxial UIV: 6.2° vs. C2 UIV: 7.4°), although these differences were statistically insignificant (P=0.664 and P=0.773, respectively). C2 UIV patients also showed a trend of greater baseline to 1Y improvement in T1 slope (subaxial UIV: 2.0° vs. C2 UIV: 7.0°, P=0.085).
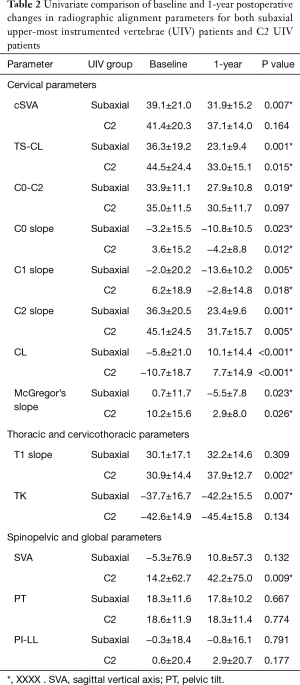
Full table
Cervical spine flexibility by UIV group
At 1Y, there were no differences between UIV groups in CL flexion (subaxial UIV: −0.2° vs. C2 UIV: 6.2°, P=0.115) or extension (subaxial UIV: 13.9° vs. C2 UIV: 9.9°, P=0.366), indicating flexibility of the cervical spine was maintained at 1Y regardless of UIV level. Similarly, there were no differences between UIV groups in 1Y upper-cervical flexibility, as assessed by C0-C2 lordosis flexion (subaxial UIV: 14.6° vs. C2 UIV: 14.4°, P=0.958) and extension (subaxial UIV: 40.2° vs. C2 UIV: 37.9°, P=0.489).
Clinical outcomes by UIV group
UIV groups did not differ in overall complication rates (subaxial UIV: 64.5% vs. C2 UIV: 67.7%, P=0.788) or rates of operative complications (subaxial UIV: 0.0% vs. C2 UIV: 16.1%, P=0.195), including dural tears (three patients), respiratory failure, dysphagia, and excessive bleeding (one patient for each). Both UIV groups had a reoperation rate of 9.7%. Indications for revision within the C2 UIV group were iatrogenic C5 radiculopathy (N=1), iatrogenic neurologic deficit (N=1), and lateral mass burst fracture (N=1); indications for revision within the subaxial group were instrumentation failure (N=1), and junctional kyphosis (N=2). No patients developed pseudarthrosis by 1Y. Baseline to 1Y changes in HRQL assessments did not differ between UIV groups (Table 3). Additionally, at 1-year postoperative, UIV groups did not differ in self-reported neck pain intensity (P=0.233) or neck-related driving disability (P=0.231), reading disability (P=0.138), sleep loss (P=0.479), or difficulty in personal care (P=0.137).
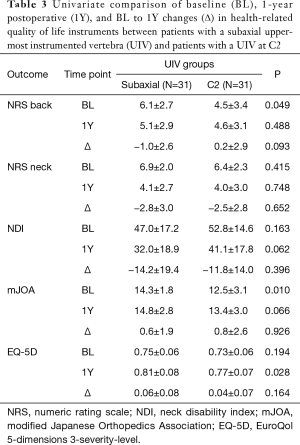
Full table
Effect of bone quality on radiographic outcomes
Eight patients included in the present study had physician-documented osteoporosis or pre-osteoporosis. Of these patients, 4 had UIV at C2, and 4 had subaxial UIV. Poor bone quality patients with C2 UIV showed significantly greater reductions in cervical and upper-CD from baseline to 1Y: TS-CL (subaxial UIV: −13.2° vs. C2 UIV: −41.7°, P=0.029) and C2 slope (subaxial UIV: −11.4° vs. C2 UIV: −45.5°, P=0.029). C2 UIV patients also showed a trend of more level McGregor’s slope at 1Y (subaxial UIV: −13.6° vs. −0.1°, P=0.057), indicating level horizontal gaze.
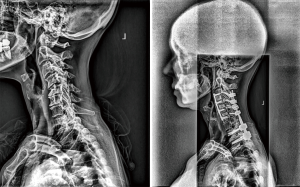
Case examples
Figures 1 and 2 present pre- and post-operative case examples of surgical CD patients with UIV at C2 and C5, respectively. Both patients presented with similar baseline cSVA (C2 UIV: 29 mm vs. subaxial UIV: 24 mm), though the C2 UIV patient presented with less severe horizontal gaze disruption, as assessed by C2 slope (C2 UIV: 20° vs. subaxial UIV: 25°). Both patients had a lower-most instrumented vertebrae at T2. Following surgery, the C2 UIV patient appreciated greater change in both cSVA (C2 UIV: −12 mm vs. subaxial UIV: 4 mm) and C2 slope (C2 UIV: −16° vs. subaxial UIV: −10°). The C2 UIV patient also showed superior improvement in NDI score (C2 UIV: −14 vs. subaxial UIV: −8). Neither patient experienced an intraoperative complication, though the subaxial UIV patient experienced a dysphagia complication, and the C2 UIV experienced a vascular complication.

Discussion
Successful operative management for CD necessitates clear surgical planning. Critical for developing a comprehensive surgical plan is a thorough assessment of both cervical sagittal and coronal alignment, cervical flexibility, neurologic deficits, patient frailty, and comorbidity status, among other factors. Despite recent advances in the development of a standardized classification system for CD, there still exists wide variation among deformity surgeons in surgical strategy, including a lack of consensus regarding surgical approach, osteotomy utilization, and fusion length (14,15). While preoperative surgical planning algorithms for CD-corrective surgery exist in the literature, they place little emphasis on optimal fusion length and UIV level (1,16). As such, the goal of this study was to evaluate differences in alignment and clinical outcomes surgical CD patients with a subaxial UIV and patients with a UIV at C2.
In UIV groups matched for similar cervical sagittal deformity, patients with instrumentation ending at C2 did not differ from subaxial UIV patients in postoperative radiographic alignment, cervical flexibility, rates of reoperation, or HRQL. Furthermore, in a subpopulation of patients with osteoporosis and pre-osteoporosis, extension of fusion constructs to C2 was associated with superior radiographic outcomes, including significant baseline to 1-year reductions in TS-CL and C2 slope, as well as more level horizontal gaze than patients with a subaxial UIV. In contrast to subaxial fixation, which typically only incorporates lateral mass screws, fixation at C2 has been shown to provide substantial stability and vertebral control, as screws may be placed in the pars, pedicle, or lamina (2,3,17,18). Our results suggest that for select CD patients, extension of the fusion construct from the subaxial spine to C2 may provide radiographic benefit, and offers comparable postoperative range of motion and clinical outcomes to subaxial fixation.
UIV groups did not differ in primary apex of deformity or baseline cervical alignment, as assessed by the common regional deformity metrics of TS-CL, cSVA, and C0-C2 lordosis. C2 UIV patients were older, however, and had significantly worse horizontal gaze at baseline, both of which may have been important factors influencing choice of UIV level. For elderly patients and patients with poor bone quality, there is evidence suggesting the need for increased points of fixation and multilevel pedicle screws to provide sufficient segmental stability (19). Indeed, as compared to subaxial UIV patients with poor bone quality, our analysis showed significantly superior cervical alignment and horizontal gaze outcomes for osteoporotic and pre-osteoporotic C2 UIV patients. These results suggest that additional fixation at C2 may be beneficial for older patients and patients with compromised bone mineral density.
Despite having significantly longer fusion constructs than subaxial UIV patients, C2 UIV patients did not differ from subaxial UIV patients in postoperative cervical range of motion. Specifically, there were no radiographic differences between UIV groups in C2−C7 lordosis flexion or extension, as well as C0−C2 flexion or extension. This is a particularly important finding, as previous research shows a significant relationship between cervical range of motion and HRQL outcomes, as well as between decreased flexion CL and increased myelopathy severity (20). While loss of cervical range of motion may be unavoidable following multilevel cervical fusion, our results show adequate cervical flexibility for patients with a C2 UIV that is comparable to the flexibility of patients with shorter and more caudal fusion constructs.
It is important to note that although the C2 UIV group had a higher intraoperative complication rate than subaxial UIV patients, this difference was not statistically significant. Furthermore, these complications were not necessarily a product of C2 fixation alone. Previous research suggests a relationship between surgical approach and complication rates in CD-corrective surgery, showing combined approaches to be associated with higher complication rates (21). Correction of more severe deformity often warrants a combined surgical approach—this trend was evident in our patient population, as C2 UIV patients presented with more severe horizontal gaze disruption and had a higher rate of combined surgical approach. C2 UIV patients also underwent surgeries involving osteotomies at a higher rate than subaxial UIV patients (55% vs. 39%), and had a significantly higher rate of surgical decompression (71% vs. 32%, P=0.002). Thus, in our analysis, the complication rate for C2 UIV patients may be explained by longer fusions and more severe baseline deformity necessitating more complex and invasive correction, not necessarily C2 fixation alone.
A key limitation of this study is the small sample size, which diminishes the statistical significance of our findings, and increases the likelihood of Type I “false positive” errors. Additionally, while our analysis controlled for differences in baseline cervical sagittal malalignment, this is not the only factor included in the preoperative calculus of UIV level. Patient-specific anatomy plays a key role in choice of UIV, with some anatomical studies showing that 20% of C2 specimens preclude pedicle screw placement due to vertebral artery anatomy and variations in pedicle width and height (22). Small sample size and limitations inherent in our database’s construction made us unable to control for these and other covariates which may have affected UIV level. The database we used also lacked an objective measure of bone density, like DEXA scan results, for example, effectively limiting our bone quality sub-analysis to only patients with physician-reported osteoporosis and pre-osteoporosis. Furthermore, all subaxial UIV fusion cases in the present analysis utilized lateral mass screws, not pedicle screws. It is possible that subaxial pedicle screw fixation, in conjunction with modern navigational techniques, may result in improved fixation and alignment outcomes—this should be a focus of future research. With these limitations in mind, our study still presents a heterogeneous patient population from multiple surgical centers across the United States, and thus offers a generalizable perspective on the influence of UIV in CD-corrective surgery.
Conclusions
Surgical CD patients with a UIV at C2 did not differ from subaxial UIV patients in 1-year postoperative cervical flexibility, HRQL outcomes, or radiographic outcomes. C2 UIV patients also showed a trend of greater baseline to 1-year improvements in horizontal gaze. Similarly, in patients with poor bone quality, a C2 UIV was associated with significantly more level horizontal gaze at 1-year, and significantly greater baseline to 1-year reductions in deformity, as assessed by TS-CL. To our knowledge, these findings represent the first specific investigation of proximal level choice in an adult CD population. For patients with a UIV at C2, realignment advantages were observed in the setting of minimal functional loss; however, further research is necessary to determine the durability of these advantages. These results can be used to further inform deformity surgeons during the surgical planning process.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: All participating centers obtained Institutional Review Board approval prior to patient enrollment. The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
- Tan LA, Daniel Riew K, Traynelis VC. Cervical spine deformity—Part 2: Management algorithm and anterior techniques. Neurosurgery 2017;81:561-7. [Crossref] [PubMed]
- Benke MT, O’Brien JR, Turner AWL, et al. Biomechanical comparison of transpedicular versus intralaminar C2 fixation in C2-C6 subaxial constructs. Spine (Phila Pa 1976) 2011;36:E33-7. [Crossref] [PubMed]
- Kimura H, Shikata J, Odate S, et al. Anterior corpectomy and fusion to C2 for cervical myelopathy: clinical results and complications. Eur Spine J 2014;23:1491-501. [Crossref] [PubMed]
- Karaikovic EE, Daubs MD, Madsen RW, et al. Morphologic characteristics of human cervical pedicles. Spine (Phila Pa 1976) 1997;22:493-500. [Crossref] [PubMed]
- Sanelli PC, Tong S, Gonzalez RG, et al. Normal variation of vertebral artery on CT angiography and its implications for diagnosis of acquired pathology. J Comput Assist Tomogr 2002;26:462-70. [Crossref] [PubMed]
- Ghori A, Le HV, Makanji H, et al. Posterior Fixation Techniques in the Subaxial Cervical Spine. Cureus 2015;7:e338. [PubMed]
- Champain S, Benchikh K, Nogier A, et al. Validation of new clinical quantitative analysis software applicable in spine orthopaedic studies. Eur Spine J 2006;15:982-91. [Crossref] [PubMed]
- Rillardon L, Levassor N, Guigui P, et al. Validation of a tool to measure pelvic and spinal parameters of sagittal balance. Rev Chir Orthop Reparatrice Appar Mot 2003;89:218-27. [PubMed]
- O’Brien MF, Kuklo TRTR, Blanke KM, et al. Spinal Deformity Study Group Radiographic Measurement Manual. Memphis, TN: Medtronic Sofamor Danek; 2005; Available online: http://www.oref.org/docs/default-source/default-document-library/sdsg-radiographic-measuremnt-manual.pdf?sfvrsn=2
- Ames CP, Blondel B, Scheer JK, et al. Cervical radiographical alignment: comprehensive assessment techniques and potential importance in cervical myelopathy. Spine (Phila Pa 1976) 2013;38:S149-60. [Crossref] [PubMed]
- Ames CP, Smith JS, Scheer JK, et al. Impact of spinopelvic alignment on decision making in deformity surgery in adults: A review. J Neurosurg Spine 2012;16:547-64. [Crossref] [PubMed]
- Lafage R, Challier V, Liabaud B, et al. Natural Head Posture in the Setting of Sagittal Spinal Deformity: Validation of Chin-Brow Vertical Angle, Slope of Line of Sight, and McGregor’s Slope With Health-Related Quality of Life. Neurosurgery 2016;79:108-15. [Crossref] [PubMed]
- Andrade C. Propensity Score Matching in Nonrandomized Studies: A Concept Simply Explained Using Antidepressant Treatment During Pregnancy as an Example. J Clin Psychiatry 2017;78:e162-5. [Crossref] [PubMed]
- Ames CP, Smith JS, Eastlack R, et al. Reliability assessment of a novel cervical spine deformity classification system. J Neurosurg Spine 2015;23:673-83. [Crossref] [PubMed]
- Smith JS, Klineberg E, Shaffrey CI, et al. Assessment of Surgical Treatment Strategies for Moderate to Severe Cervical Spinal Deformity Reveals Marked Variation in Approaches, Osteotomies, and Fusion Levels. World Neurosurg 2016;91:228-37. [Crossref] [PubMed]
- Hann S, Chalouhi N, Madineni R, et al. An algorithmic strategy for selecting a surgical approach in cervical deformity correction. Neurosurg Focus 2014;36:E5. [Crossref] [PubMed]
- Tan LA, Riew KD, Traynelis VC. Cervical Spine Deformity—Part 3: Posterior Techniques, Clinical Outcome, and Complications. Neurosurgery 2017;81:893-8. [Crossref] [PubMed]
- Kurd MF, Millhouse PW, Schroeder GD, et al. Lateral Mass Fixation in the Subaxial Cervical Spine. J Spinal Disord Tech 2015;28:259-63. [Crossref] [PubMed]
- Goldstein CL, Brodke DS, Choma TJ. Surgical Management of Spinal Conditions in the Elderly Osteoporotic Spine. Neurosurgery 2015;77 Suppl 4:S98-107. [Crossref] [PubMed]
- Liu S, Lafage R, Smith JS, et al. The Impact of Dynamic Alignment, Motion, and Center of Rotation on Myelopathy Grade and Regional Disability in Cervical Spondylotic Myelopathy. In: International Meeting on Advanced Spine Techniques (IMAST); July 16-19. Valencia, Spain, United States; 2014:690-700.
- Smith JS, Ramchandran S, Lafage V, et al. Prospective Multicenter Assessment of Early Complication Rates Associated With Adult Cervical Deformity Surgery in 78 Patients. Neurosurgery 2016;79:378-88. [Crossref] [PubMed]
- Igarashi T, Kikuchi S, Sato K, et al. Anatomic study of the axis for surgical planning of transarticular screw fixation. Clin Orthop Relat Res 2003.162-6. [Crossref] [PubMed]


