
Outcomes of surgical intervention for degenerative lumbar spondylolisthesis: a comparative analysis of different surgical fixation techniques
Highlight box
Key findings
• Both PLIF and TLIF result in clinically significant improvements in disability, back and leg pain for degenerative lumbar spondylolisthesis, with superiority of TLIF for improvements in back and leg pain.
What is known and what is new?
• Studies support both PLIF or TLIF as preferred surgical approaches for degenerative lumbar spondylolisthesis. Lack of consensus regarding effectiveness means scant data regarding cost effectiveness, surgical operative time, resources, patient hospital stay and recovery; particularly in the medium term.
• This study shows that TLIF demonstrated better improvement in back and leg pain outcomes.
What is the implication, and what should change now?
• Interbody fusion using either PLIF or TLIF provides good outcomes for adult degenerative lumbar spondylolisthesis.
• TLIF offers a useful alternative to surgeons with better back and leg pain outcomes to the more traditional PLIF procedure.
Introduction
Degenerative lumbar spondylolisthesis is a common condition that can result in pain, disability, and reduced quality of life (1). The incidence of spondylolysis is approximately 3% to 6% in the general population (2). The prevalence is higher (12%) in adolescents, athletes, and gymnasts (3). The treatment for spondylolisthesis is still a huge challenge as the aetiology of this disease is multifaceted and not yet fully understood (4). Most patients undergoing treatment for spondylolisthesis are currently managed conservatively (5). Only when conservative treatment has been deemed unsuccessful is surgical treatment recommended (6). Due to potential instability, spinal fusion is recommended. Indication for spinal fusion may include discogenic/facetogenic low back pain, neurogenic claudication, radiculopathy due to foraminal stenosis, lumbar degenerative spinal deformity including symptomatic spondylolisthesis and degenerative scoliosis (7).
The two most commonly used techniques for lumbar spinal fusion surgery, both using a posterior approach are transforaminal lumbar interbody fusion (TLIF) and posterior lumbar interbody fusion (PLIF); the PLIF uses a bilateral route whereas the TLIF uses a unilateral route (8). Occasionally, the lumbar spine is fused without interbody cage or grafting, where fusion is attempted at the facet joint or nearby outer aspect of vertebra (9). It is important to know whether either technique provides better clinical outcomes, has fewer complications, or is more cost effective. Limited data exist. A small prospective observational study recruited 21 patients with grades 1 and 2 spondylolisthesis, comparing outcomes for TLIF (n=10) and PLIF (n=11) at 1-, 3-, and 6-month post-surgery (10). This is the only study investigating outcomes in the mid-term (6 months). Results illustrated that both techniques (within group analyses) demonstrated significant improvements in pain [Visual Analogue Scale, (VAS)] and Oswestry Disability Index (ODI) at all timepoints compared to baseline, but with no statistical differences between the techniques (10). Most existing studies are retrospective in nature. Two recent small retrospective observational studies compared TLIF and PLIF for patients with degenerative spondylolisthesis undergoing single level surgery measuring outcome at 2 years following surgery. Kim et al. [2018] (11) recruited 99 patients (n=62 TLIF, n=37 PLIF) and found no differences between groups at 2 years for ODI, Numerical Rating Scale (NRS) back pain, NRS leg pain, quality of life (EQ5D) and direct/indirect and total costs. Kim et al. (11) did observe a statistically significant difference for change scores (baseline to 2 years) in back pain and the physical component score of the SF12, favouring TLIF. Kelly et al. [2019] (12) recruited 119 patients (n=544 TLIF, n=285 PLIF) and found no difference in improvement of ODI at 2 years (P=0.97). Complication and reoperation rates were comparable apart from dural tears being more common for PLIF (P<0.01). Costs were higher for TLIF for implants (P<0.01) and operation time (P=0.01) (12). A further small study (n=56; n=24 TLIF, n=32 PLIF) by Fujimori et al. (13) demonstrated statistically significant differences between techniques for VAS back pain and VAS leg pain change scores at a minimum of 1 year follow-up compared to baseline, with greater improvements for TLIF; but not for VAS back pain or VAS leg pain at follow-up. There were no differences for ODI or function. A further recent retrospective study (Liu et al., 2016) compared outcomes in the short term in 226 patients (1 week after surgery), again finding within group improvements for both techniques for pain (VAS) and functional outcomes but no differences between groups (14). However, Liu and colleagues [2016] did not distinguish back and leg pain. For all of these studies, within group improvements were significant showing benefit of surgery but there were no between group differences at the point of measuring outcome, with one small study evaluating mid-term outcomes. Since there is increasing demand for shorter hospital stay, early return to work and reducing postoperative morbidity (15), an adequately powered low risk of bias observational study measuring outcomes at 6 months is required to further inform decision-making regarding surgery.
The present study aims firstly to investigate whether there is a difference in clinical outcomes (pain, disability and quality of life) and complication rates following PLIF and TLIF for degenerative lumbar spondylolisthesis (Objectives 1 and 2). Secondly, we compared PLIF and TLIF approaches for cost effectiveness of treatment of degenerative lumbar spondylolisthesis (Objective 3). We present the following article in accordance with the STROBE reporting checklist (available at https://jss.amegroups.com/article/view/10.21037/jss-22-24/rc) to ensure quality of design and reporting (16).
Methods
Study design
An observational retrospective cohort study using data from the British Spine Registry (BSR).
Data source
Data were obtained from the BSR registry database. The BSR is an automated web-based database established to record data about spinal surgery in the UK. BSR was launched in 2012 by the British Association of Spine surgeons to monitor the outcome of spinal procedure. The BSR collates large volume of clinical and patient outcome data following surgery for spinal deformity, and degenerative spinal conditions, trauma, infection and intradural tumour. This study accessed all data collected through the lumbar degenerative pathway. The Patient Reported Outcome Measures (PROMs) in the lumbar degenerative pathway include back and leg pain measured using the NRS, ODI and the Euro-QOL five dimensions questionnaire (ED-5D 5L). Questionnaires are entered manually if completed on paper or electronically by patients through kiosks in clinic or email links.
Population
Inclusion criteria
Adult patients aged (≥18 years) who underwent surgical fixation for degenerative lumbar spondylolisthesis with recorded pre- and post-operative outcomes scores at 6 months.
Exclusion criteria
Patients diagnosed with spinal fracture, malignancy or infection, or previous degenerative lumbar spondylolisthesis surgery.
Outcome
Outcome analysed included an individual’s change in pain, disability, and quality of life from baseline measured using PROMS [EQ-5D 5L, VAS (back and leg), ODI]. Outcome was measured at 6 months post-surgery. Difference in outcome were expressed in mean ± standard deviation.
Demographic, clinical, and surgical variables
Data for the following variables were extracted: age, gender, comorbidities, body mass index (BMI), smoking status, education, analgesia, ODI, walking distance, procedure (TLIF, PLIF), degenerative spondylolisthesis grade, American Society of Anaesthesiologist (ASA) grade (self-report overall health), instrumentation, complications (e.g., loss of bowel and bladder control), blood loss, operative time, and current work status/days post-surgery when returned to work/normal function.
Ethical statement
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Ethical approval for this study was obtained from the University of Birmingham Research Ethics Committee (No. ERN_19-1274AP3). Patients provided consent for their data to be used for evaluation purposes when they initially sign up for the registry. Following listing for surgery patients are offered the option to participate in the registry data collection and are consented at this point. Prior to the scheduled operation, patients are asked to fill in a pre-operative questionnaire, and then at a series of time points post-surgery. Patients can withdraw from the registry at any point. Personal details such as name, address, phone number and email address are captured with patient’s consent in addition to details of diagnosis, operation, and complication. However, no personal data were shared as part of this project, and data were managed/analysed in an anonymised format.
Missing data
Variables such as BMI, alcohol intake (male/female), work status, job type, work type, education, smoking status, previous treatment for back pain and both spondylolisthesis and ASA grades were missing. For this study missing data were managed by categorising the missing values. For categorical variable (e.g., smoking status) and continuous variable (e.g., BMI) a separate missing category was created for those with missing data.
Statistical analysis
Descriptive statistics
All statistical analyses were conducted using STATA version 13.1 (Stata Corp., College Station Texas, USA). Descriptive statistics were used to summarise participants’ characteristics. For descriptive analyses, means, standard deviation (SD), medians and interquartile range (IQR) for continuous variables and frequencies for categorical variables were calculated. Variability of distribution for each variable was tested separately. For data with high skewness, the distribution was tested using histograms, medians and IQR was used to describe the central tendency and variability of the data.
Analysis of PROMS—pre- and post-surgical intervention
Participants were categorised according to the surgical fixation techniques: TLIF and PLIF. Mann Whitney sum rank test was used to compare changes in PROMs, surgical data and costs at 6 months follow-up for each surgical technique. A P value of (<0.05) with a confidence interval of 95% was considered significant.
Results
Characteristics of the study population
The study population consists of 1,838 patients. A descriptive analysis of the baseline data are provided in Table 1. The mean age at baseline was 61.8±12.4 years for those who underwent PLIF and 61.1±12.4 years for TLIF. This surgery was more likely to be the first surgical procedure for PLIF (92.5%) and 90.1% for patients who underwent TLIF. Some data were missing, for example information on job type was missing (92.6% PLIF, 95.6% TLIF) and so it was not possible to interpret. Twenty-four patients (4.8%) in the PLIF group and 109 patients (8.2%) in the TLIF group had grade 1 spondylolisthesis, compared to 21 (4.2%) in the PLIF group and 61 (4.6%) in the TLIF group who had grade 2 spondylolisthesis. Among PLIF patients, 55.3% reported ASA grade 2 status. Conversely, 60.7% of TLIF patients reported ASA grade 2 status. The mean pre-operative ODI was 45.1±1.30 and 51.1±0.90 for patients who underwent PLIF and TLIF respectively; mean pre-operative NRS (back pain) was 6.67±2.18 and 7.02±2.28. Mean pre-operative NRS (leg pain) was 6.68±2.58 and 6.48±2.93. The mean pre-operative EQ-5D-5L–Health VAS was 55.61±23.21 and 54.50±24.60 for PLIF and TLIF respectively. Similarly, the mean pre-operative EQ-5D-5L score was 0.41±0.24 and 0.31±0.30 for PLIF and TLIF. Most patients in PLIF (44.6%) and TLIF group (46.1%) had interbody fusion level L4/5.
Table 1
| Variables | PLIF [n=505 (27.5%)] | TLIF [n=1,333 (72.5%)] |
|---|---|---|
| Age (years), mean ± SD | 61.8±12.4 | 61.1±12.4 |
| Age categories (years), n (%) | ||
| <20 | 5 (1.0) | 1 (0.1) |
| 20–29.9 | 3 (0.6) | 12 (0.9) |
| 30–39.9 | 28 (5.5) | 61 (4.6) |
| 40–49.9 | 63 (12.5) | 143 (10.7) |
| 50–59.9 | 132 (26.1) | 312 (23.4) |
| ≥60 | 274 (54.3) | 804 (60.3) |
| Gender, n (%) | ||
| Female | 293 (57.6) | 827 (61.6) |
| BMI (kg/m2), median [IQR] | ||
| Baseline | 27.6 [23.7, 30.6] | 28.1 [25.3, 32.1] |
| BMI (kg/m2), categories, baseline, n (%) | ||
| <20 | 3 (0.6) | 17 (1.3) |
| 20–24.9 | 38 (7.5) | 67 (5.0) |
| 25–29.9 | 42 (8.3) | 150 (11.3) |
| 30–34.9 | 24 (4.8) | 82 (6.2) |
| 35–39.9 | 9 (1.8) | 41 (3.1) |
| ≥40 | 4 (0.8) | 10 (0.8) |
| Not reported | 385 (76.2) | 966 (72.5) |
| Number of surgical procedures, n (%) | ||
| 1 | 467 (92.5) | 1,200 (90.1) |
| 2 | 27 (5.3) | 99 (7.4) |
| 3 | 7 (1.4) | 28 (2.1) |
| 4 | 4 (0.8) | 6 (0.5) |
| Alcohol intake—female, n (%) | ||
| 1–21 units per week | 6 (2.0) | 21 (2.5) |
| 22–34 units per week | 2 (0.7) | 0 (0.0) |
| More than 35 units per week | 1 (0.3) | 0 (0.0) |
| None | 3 (1.1) | 7 (0.9) |
| Not reported | 281 (95.9) | 799 (96.6) |
| Alcohol intake—male, n (%) | ||
| 1–28 units per week | 7 (3.3) | 12 (2.4) |
| 29–49 units per week | 1 (0.5) | 1 (0.2) |
| None | 1 (0.5) | 5 (1.0) |
| Not reported | 203 (95.7) | 488 (96.4) |
| Work status, n (%) | ||
| Off work | 15 (3.0) | 23 (1.7) |
| Retired | 15 (3.0) | 50 (3.8) |
| Student | 2 (0.4) | 0 (0.0) |
| Unemployed | 0 (0.0) | 4 (0.3) |
| Not reported | 473 (93.6) | 1,256 (94.2) |
| Job type, n (%) | ||
| Full time | 20 (4) | 34 (2.6) |
| Part time | 17 (3.4) | 24 (1.8) |
| Not reported | 468 (92.6) | 1,275 (95.6) |
| Work type, n (%) | ||
| Desk bound | 16 (3.2) | 23 (1.7) |
| Manual | 9 (1.8) | 17 (1.3) |
| Manual desk | 11 (2.2) | 17 (1.3) |
| Not reported | 469 (92.8) | 1,276 (95.7) |
| Education, n (%) | ||
| Less than secondary education | 1 (0.2) | 1 (0.1) |
| Postgraduate | 9 (1.8) | 8 (0.6) |
| Secondary education | 30 (5.9) | 57 (4.3) |
| Undergraduate | 9 (1.8) | 28 (2.1) |
| Higher education | 20 (4.0) | 45 (3.4) |
| Not reported | 436 (86.3) | 1,194 (89.5) |
| Smoking status, n (%) | ||
| Smoker | 9 (1.8) | 19 (1.4) |
| Non-smoker | 60 (11.9) | 121 (9.1) |
| Not reported | 436 (86.3) | 1,193 (89.5) |
| Medication, n (%) | ||
| Ace-inhibitor | 0 (0.0) | 1 (0.1) |
| Antidepressant | 0 (0.0) | 3 (0.2) |
| NSAID | 0 (0.0) | 1 (0.1) |
| Opioid analgesic | 3 (0.6) | 8 (0.6) |
| Proton pump inhibitor | 0 (0.0) | 1 (0.1) |
| No medication prescribed | 502 (99.4) | 1,319 (98.9) |
| Previous treatment for back, n (%) | ||
| Yes | 11 (2.2) | 22 (1.7) |
| No | 57 (11.3) | 112 (8.4) |
| Not reported | 437 (86.5) | 1,199 (89.9) |
| Spondylolisthesis grade, n (%) | ||
| I | 24 (4.8) | 109 (8.2) |
| II | 21 (4.2) | 61 (4.6) |
| III | 1 (0.2) | 7 (0.5) |
| IV | 1 (0.2) | 0 (0.0) |
| V | 1 (0.2) | 0 (0.0) |
| Not reported | 457 (90.4) | 1,156 (86.7) |
| ASA grade, n (%) | ||
| 1 | 163 (34.7) | 362 (28.4) |
| 2 | 260 (55.3) | 773 (60.7) |
| 3 | 47 (10.0) | 138 (10.8) |
| 4 | 0 (0.0) | 1 (0.1) |
| Not reported | 35 (6.9) | 59 (4.4) |
| ODI (disability), mean ± SD | ||
| Baseline | 45.1±1.30 | 51.1±0.90 |
| Baseline data completeness, n (%) | 1,132 (60.3) | |
| Missing, n (%) | 706 (38.4) | |
| NRS (back pain), mean ± SD | ||
| Baseline | 6.7±2.2 | 7.1±2.3 |
| Baseline data completeness, n (%) | 1,156 (61.2) | |
| Missing, n (%) | 682 (37.1) | |
| NRS (leg pain), mean ± SD | ||
| Baseline | 6.8±2.6 | 6.5±2.9 |
| Baseline data completeness, n (%) | 1,156 (61.2) | |
| Missing, n (%) | 682 (37.1) | |
| EQ-5D-5L–Health/VAS, mean ± SD | ||
| Baseline | 55.6±23.2 | 54.5±24.6 |
| Baseline data completeness, n (%) | 1,096 (58.4) | |
| Missing, n (%) | 742 (41.1) | |
| EQ-5D-5L, mean ± SD | ||
| Baseline | 0.41±0.24 | 0.31±0.30 |
| Baseline data completeness, n (%) | 1,098 (58.5) | |
| Missing, n (%) | 740 (41.1) | |
| Surgical level, n (%) | ||
| L2/3 | 3 (0.6) | 9 (0.7) |
| L2/3 – L3/4 | 3 (0.6) | 1 (0.1) |
| L3/4 | 36 (7.1) | 87 (6.5) |
| L3/4 – L4/5 | 21 (4.2) | 34 (2.6) |
| L3/4 –L4/5 – L5/S1 | 1 (0.2) | 2 (0.2) |
| L3/4 – L5/S1 | 1 (0.2) | |
| L4/5 | 225 (44.6) | 615 (46.1) |
| L4/5 – L3/4 | 5 (1.0) | 12 (0.9) |
| L4/5 – L5/S1 | 27 (5.3) | 74 (5.6) |
| L5/S1 | 142 (28.1) | 348 (26.1) |
| L5/S1- L3/4- L4/5 | 1 (0.2) | 9 (0.7) |
| L5/S1 – L4/5 | 17 (3.4) | 69 (5.2) |
| L2/3 – L3/4 – L4/5 | 2 (0.2) | |
| L2/3 – L3/4 – L4/5 – L5/S1 | 1 (0.1) | |
| L2/3 – L4/5 | 1 (0.1) | |
| L4/5 – L2/3 – L3/4 | 3 (0.2) | |
| L4/5 – L5/S1 – L2/3 – L3/4 | 4 (0.3) | |
| L4/5 – L5/S1 – L3/4 | 3 (0.2) | |
| L5/S1 – L2/3 – L3/4 – L4/5 | 1 (0.1) | |
| L5/S1 – L3/4 | 2 (0.2) | |
| Not reported | 23 (4.6) | 56 (4.2) |
PLIF, posterior lumbar interbody fusion; TLIF, transforaminal lumbar interbody fusion; NSAID, non-steroidal anti-inflammatory drugs; BMI, body mass index; ODI, Oswestry Disability Index; NRS, Numerical Rating Scale; VAS, Visual Analogue Scale; ASA, American Society of Anesthesiologists.
Objective 1: to compare the clinical outcomes (pain, disability, and quality of life) following different surgical fixation interventions for degenerative lumbar spondylolisthesis
The results did not demonstrate a statistically significant or clinically significant difference in the functional outcomes as measured by the ODI between PLIF and TLIF groups at 6 months follow-up (P=0.620). NRS (back and leg) demonstrated a statistically significant difference. Quality of life scores measured by EQ-5D-5L–Health (VAS) and EQ-5D-5L did not demonstrate a statistically significant difference. There was a significant difference between groups at baseline for ODI (Table 2). The ODI improvement (change) at 6 months from baseline in each group was the same for the two surgical interventions (PLIF: 20.1±20.2; TLIF: 21.1±18.9). There was no statistically significant difference between the two groups (P=0.620) (Figure 1).
Table 2
| Patient reported outcome | PLIF [mean (SD)] | TLIF [mean (SD)] | P value (between groups) |
|---|---|---|---|
| ODI | |||
| Pre-operative | 45.1±1.30 | 51.1±0.90 | <0.001 |
| 6 months post-operative | 24.1±1.80 | 31.1±1.16 | 0.002 |
| Change (pre – 6 months post-operative) | 20.1±20.2 | 21.1±18.9 | 0.620 |
| NRS (back pain) | |||
| Pre-operative | 6.67±2.18 | 7.02±2.28 | 0.112 |
| 6 months post-operative | 2.62±2.56 | 3.58±2.86 | <0.001 |
| Change (pre – 6 months post-operative) | 4.04±3.06 | 3.43±3.14 | 0.048 |
| NRS (leg pain) | |||
| Pre-operative | 6.68±2.58 | 6.48±2.93 | 0.474 |
| 6 months post-operative | 1.80±2.64 | 2.61±3.00 | 0.005 |
| Change (pre – 6 months post-operative) | 4.89±3.24 | 3.87±3.81 | 0.005 |
| EQ-5D-5L–Health VAS | |||
| Pre-operative | 55.61±23.21 | 54.50±24.60 | 0.648 |
| 6 months post-operative | 74.16±23.52 | 68.51±23.62 | 0.018 |
| Change (pre – 6 months post-operative) | −18.54±31.50 | −14.01±29.40 | 0.136 |
| EQ-5D-5L | |||
| Pre-operative | 0.41±0.24 | 0.31±0.30 | 0.001 |
| 6 months post-operative | 0.68±0.24 | 0.59±0.30 | <0.001 |
| Change (pre – 6 months post-operative) | −0.27±0.31 | −0.28±0.27 | 0.655 |
PLIF, posterior lumbar interbody fusion; TLIF; transforaminal lumbar interbody fusion; ODI, Oswestry Disability Index; NRS, Numerical Rating Scale; VAS, Visual Analogue Scale.
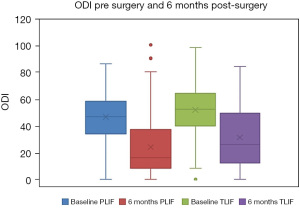
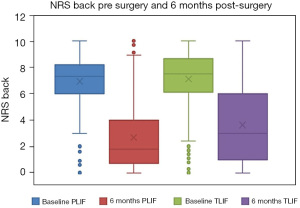
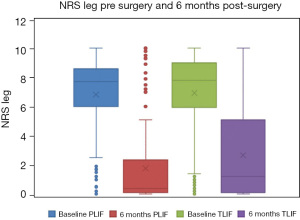
Post-operative NRS (back) scores were not statistically different between groups at baseline but significantly different at 6 months follow-up (Table 2). The NRS (back) improvements (change) at 6 months from baseline in each group were different for the two surgical interventions (PLIF: 4.04±3.06; TLIF: 3.43±3.14) and statistically significant (P=0.048) (Figure 2). Post-operative NRS (leg) scores were not statistically different between groups at baseline but significantly different at 6 months follow-up (Table 2). The NRS (leg) improvements (change) at 6 months from baseline in each group were different for the two surgical interventions (PLIF: 4.89±3.24; TLIF: 3.87±3.81), and statistically significant (P=0.005) (Figure 3). Post-operative EQ-5D-5L–Health (VAS) scores were not statistically different between groups at baseline but significantly different at 6 months follow-up (Table 2). The EQ-5D-5L–Health (VAS) improvement (change) at 6 months from baseline in each group were similar for the two surgical interventions (PLIF: −18.54±31.50; TLIF: −14.01±29.40), and not statistically significant (P=0.136) (Figure 4).
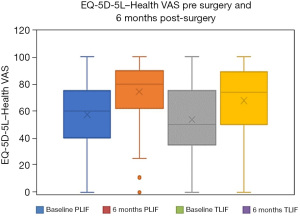
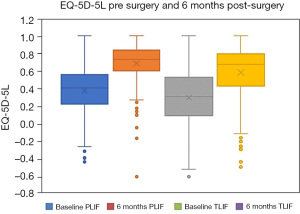
There was a significant difference between groups at baseline. Post-operative EQ-5D-5L scores were statistically different between groups (Table 2). The EQ-5D-5L improvement (change) at 6 months from baseline in each group was the same for the two surgical interventions (PLIF: −0.27±0.31; TLIF: −0.28±0.27), and not statistically significant (P=0.655) (Figure 5).
Objective 2: to compare rate of complications between PLIF and TLIF
Peri-operative complication data are reported in Table 3. For most patients there were no reported intra-operative problems, 90.1% for PLIF and 92.3% for TLIF. Blood loss was significantly different between PLIF and TLIF (P=0.04). There were no differences for intra-operative problems and ASA grade between TLIF and PLIF. Intra-operative complications in relation to L4/5 interbody fusion shows greater complication associated with PLIF intervention: dural tear 6.3% compared to 4.2% and excessive bleeding 1.3% compared to 0.5% for those undergoing TLIF (Table S1).
Table 3
| Variables | PLIF [n=505 (26.8%)] | TLIF [n=1,333 (70.6%)] | P value |
|---|---|---|---|
| Estimated blood loss (mL) (+1 SD) | 380±374 | 311±298 | 0.041 |
| Intra-operative complications, n (%) | 0.706 | ||
| Cardiac problems | 0 (0.0) | 1 (0.1) | |
| Dural tear | 28 (5.7) | 57 (4.4) | |
| Excessive bleeding | 6 (1.2) | 9 (0.7) | |
| Implant malposition | 6 (1.2) | 14 (1.1) | |
| Nerve injury | 2 (0.4) | 2 (0.2) | |
| Peripheral neuropraxia | 1 (0.2) | 1 (0.1) | |
| Radicular pain weakness | 0 (0.0) | 3 (0.2) | |
| Vascular injury | 0 (0.0) | 1 (0.1) | |
| None | 445 (90.1) | 1,206 (92.3) | |
| Other complications | 6 (1.2) | 13 (1.0) | |
| Bleeding haematoma, n (%) | 0 (0.0) | 1 (0.07) | 1 |
| Recurrent radiculopathy, n (%) | 0 (0.0) | 1 (0.07) | 1 |
| ASA grade, n (%) | 0.081 | ||
| 1 | 163 (34.7) | 362 (28.4) | |
| 2 | 260 (55.3) | 773 (60.7) | |
| 3 | 47 (10.0) | 138 (10.8) | |
| 4 | 0 (0.0) | 1 (0.1) |
PLIF, posterior lumbar interbody fusion; TLIF, transforaminal lumbar interbody fusion; SD, standard deviation; ASA, American Society of Anesthesiologists.
Objective 3: to compare PLIF and TLIF for cost effectiveness of treatment of degenerative lumbar spondylolisthesis
The operative time was statistically longer for PLIF (200±72 minutes) compared to TLIF (184±78) (P=0.031). Costs of implants (GB£ 2,664±1,788) and cost of consumables (GB£ 288±474) were higher for TLIF (Table 4), with costs for implants statistically different.
Table 4
| Costs | PLIF [mean (SD)] | TLIF [mean (SD)] | P value |
|---|---|---|---|
| Implant costs (GB£) | 1,298±1,620 | 2,664±1,788 | <0.001 |
| Cost of consumables (GB£) | 123±438 | 288±474 | 0.233 |
| Theatre room (minutes) | 200±72 | 184±78 | 0.031 |
PLIF, posterior lumbar interbody fusion; TLIF, transforaminal lumbar interbody fusion; SD, standard deviation.
Discussion
Lumbar interbody fusion is an established treatment for a range of spinal disorders and is performed using five main approaches; PLIF, TLIF, oblique lumbar interbody fusion (OLIF), anterior lumbar interbody fusion (ALIF) and lateral lumbar interbody fusion (LLIF). There is minimal evidence to suggest that one approach is superior to another in terms of fusion or clinical outcomes (7). OLIF is a surgical technique which is minimally invasive which uses a single port to access the disc space thus minimises damage to the muscles and ligaments (17). ALIF is similar to PLIF but is performed from the anterior (front) of the body through a small incision in the lower abdomen. This procedure requires blood vessels to be moved and the disc removed and replaced with a large cage (18). LLIF is another minimally invasive lumbar interbody fusion surgery in which access to the spine is gained from the side and involves removing the disc between two vertebrae and replacing it with an implant (19).
These results demonstrate that both PLIF and TLIF surgical techniques contributed to improved clinical outcomes that are clinically significant >Minimally Clinically Important Difference (MCID) for ODI and NRS back pain and NRS leg pain (≥1.7 reduction NRS, ≥14.3 reduction ODI) (20); representing the smallest improvement in outcome scores considered clinically meaningful by patients and clinicians (21). Results did not show a statistically or clinically significance difference for the ODI comparing PLIF and TLIF at 6 months follow-up (P=0.620). These results concur with previous findings (11,12). However, there was a significant different between groups at baseline for ODI, suggesting that ODI was a key factor influencing choice of surgical technique. The finding of no difference between groups for change at 6 months is therefore important; suggesting that surgeon decision-making for surgical technique is effective; and explains previous results (11,12). The results did demonstrate statistically and clinically meaningful differences between PLIF and TLIF in both back (P=0.048) and leg pain (P=0.005) at 6 months. Higher NRS scores (back/leg) at follow-up indicates greater pain intensity. TLIF shows greater improvement in both back and leg pain 6 months post-operatively. This is in contrast to most of the existing literature where no significant difference between techniques has been found (10-12,14). Similarly, Fujimori and colleagues reported better leg pain postoperatively for TLIF compared to PLIF although this was in the longer-term (>1 year follow-up) (13). TLIF shows greater improvement in leg/back pain compared to PLIF because of effective and durable restoration of disc height and neuroforaminal height, reduction in slippage, greater lumbar lordosis, and higher union rate which might be expected to result in reduce pain scores (22). However, no difference in quality-of-life improvement was found between PLIF and TLIF at 6 months follow-up (P=0.655). However, some of the PROMs were improved following TLIF compared to PLIF. This may be because of the minimally invasive procedure TLIF offers with equivalent postoperative fusion rates compared to PLIF; minimising the amount of iatrogenic injury to the spinal muscles. These findings are congruent with recent studies evaluating outcomes of minimally invasive spine procedures (23-25).
In this study, PLIF was associated with significantly higher blood loss (380 mL) compared to TLIF (311 mL); consistent with Liu et al.’s findings (14). A plausible reason for the greater blood loss for the PLIF surgical technique might be the longer operation times. Patel and colleagues (26) compared blood loss, surgical complications and duration of hospital stay in patients undergoing PLIF or TLIF and also found that patients undergoing PLIF were more likely to have greater blood loss (OR: 4.2; 95% CI: 3.3 to 5.3), compared to those undergoing TLIF. Intraoperative complication are common surgical problems associated with PLIF and TLIF procedures, with reported rates of complication ranging from 8% and 80% (27). The rates of surgical complications reported in this study were relatively low. However, dural tear rate was relevant for both techniques (5.7%, n=505 for PLIF; 4.4%, n=1,333 for TLIF). Among 56 patients, Fujimoro and colleagues found 12.5% dural tears following PLIF compared to 4% following TLIF (13). When considering implant cost, there was a statistically significant difference between the groups (P<0.001). Implant cost was considerably higher for the TLIF technique (£2,668) compared to the PLIF (£1,298). On the other hand, theatre time was slightly higher for PLIF (200 minutes on average) compared to 184 minutes on average for TLIF (P=0.031). It is difficult to compare costs across studies owing to limited studies evaluating cost, but these findings differ to previous studies that did not find a difference between PLIF and TLIF (11,28); but are perhaps explained by Kelly et al.’s [2019] finding that costs were higher for TLIF for implants (P<0.01) (12).
Several studies demonstrated that surgical interventions such as PLIF/TLIF improves pain and quality of life in patients affected by degenerative lumbar spondylolisthesis (Rezk et al., 2019; Zhang et al., 2008). In a retrospective case series aiming to compare the surgical outcome of PLIF and TLIF in the treatment of degenerative spondylolisthesis, Rezk et al. [2019] recruited 94 patients who underwent lumbar interbody fusion between March 2015 and May 2018. Results indicate that back pain/disability and complication rates were significantly lower in the TLIF group compared the PLIF group (29). Conversely, Zhang et al. [2017] compared operative blood loss, surgical time, length of hospital stay, pain, disability, creatinine kinase (CK) level, and complications between TLIF and PLIF for spondylolisthesis. A cohort of (26 TLIF and 29 PLIF) patients were reviewed between March 2012 and March 2014, who were managed surgically for spondylolisthesis. Results show that compared with PLIF, TLIF achieved similar reduction and fusion results with improved quality of life, shorter hospital stays, less estimated blood loss, and shorter operative times (30). Our findings are consistent with other studies suggesting that TLIF provides better post-operative outcome compared to PLIF in the short-term. Compared with other studies, this study presents a very heterogeneous population with respect to age, procedure level and demographic data. Also, the large sample size allows for more precise estimate of the surgical effect and post-surgical outcome and broadly provide a good representativeness of the sample and generalisability of the results.
Strengths and limitations
The strengths of this study are its rigorous methods and large sample size. One limitation of this study is missing data, for example for BMI. Missingness was assessed by categorising the relevant data for clear reporting. Since data not reported were nearly the same for both groups, we can assume that the results would be the same if there had been fewer data not reported in this registry. Retrospective database studies have inherent limitations. Discrepancies between data collection and data entry incur some time lag. Although the findings use retrospective data, we have nevertheless provided reliable pain, disability and cost estimates pertaining to the effectiveness of PLIF versus TLIF techniques. While important, we hope that this is at least partially compensated through the large sample size afforded by the retrospective dataset. Further analysis of hospital stay and details of rehabilitation would be advantageous to fully understand costs.
Conclusions
This study has demonstrated that both PLIF and TLIF result in clinically significant improvements in ODI, NRS back pain and NRS leg pain, with superiority of TLIF for improvements in back and leg pain. Surgeons appeared to use ODI preoperatively to decide intervention with comparable improvements for both approaches. Blood loss volume was higher for PLIF. Factors like implant costs and costs of consumables were higher for TLIF but average theatre time was higher for PLIF.
Acknowledgments
Funding: Partial funding support for this study was provided for Research Fellow time (FK) to analyse and present the data by Amplitude Clinical—the company that provides the platform hosting the British Spine Registry.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jss.amegroups.com/article/view/10.21037/jss-22-24/rc
Data Sharing Statement: Available at https://jss.amegroups.com/article/view/10.21037/jss-22-24/dss
Peer Review File: Available at https://jss.amegroups.com/article/view/10.21037/jss-22-24/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jss.amegroups.com/article/view/10.21037/jss-22-24/coif). The authors report that partial funding support for this study was provided for Research Fellow time (FK) to analyse and present the data by Amplitude Clinical—the company that provides the platform hosting the British Spine Registry. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Ethical approval for this study was obtained from the University of Birmingham Research Ethics Committee (No. ERN_19-1274AP3). Patients provided consent for their data to be used for evaluation purposes when they initially sign up for the registry.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Parker SL, Godil SS, Mendenhall SK, et al. Two-year comprehensive medical management of degenerative lumbar spine disease (lumbar spondylolisthesis, stenosis, or disc herniation): a value analysis of cost, pain, disability, and quality of life: clinical article. J Neurosurg Spine 2014;21:143-9. [Crossref] [PubMed]
- Cassas KJ, Cassettari-Wayhs A. Childhood and adolescent sports-related overuse injuries. Am Fam Physician 2006;73:1014-22.
- Simmonds AM, Rampersaud YR, Dvorak MF, et al. Defining the inherent stability of degenerative spondylolisthesis: a systematic review. J Neurosurg Spine 2015;23:178-89. [Crossref] [PubMed]
- Rihn JA, Hilibrand AS, Zhao W, et al. Effectiveness of Surgery for Lumbar Stenosis and Degenerative Spondylolisthesis in the Octogenarian Population. J Bone Joint Surg Am 2015;97:177-85. [Crossref] [PubMed]
- Backstrom KM, Whitman JM, Flynn TW. Lumbar spinal stenosis-diagnosis and management of the aging spine. Man Ther 2011;16:308-17. [Crossref] [PubMed]
- Samuel AM, Moore HG, Cunningham ME. Treatment for Degenerative Lumbar Spondylolisthesis: Current Concepts and New Evidence. Curr Rev Musculoskelet Med 2017;10:521-9. [Crossref] [PubMed]
- Mobbs RJ, Phan K, Malham G, et al. Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. J Spine Surg 2015;1:2-18. [Crossref] [PubMed]
- Cole CD, McCall TD, Schmidt MH, et al. Comparison of low back fusion techniques: transforaminal lumbar interbody fusion (TLIF) or posterior lumbar interbody fusion (PLIF) approaches. Curr Rev Musculoskelet Med 2009;2:118-26. [Crossref] [PubMed]
- Lumbar Interbody Fusion. Available online: https://www.mumbaispineclinic.com/lumbar-interbody-fusion/. Accessed (23rd September 2022).
- El-Sayed AA, El-Qazaz MY, Mohamed KE, et al. Evaluation of transforaminal lumbar interbody fusion versus posterior lumbar interbody fusion in patients of lumbar instability submitted to transpedicular screws fixation. Med J Cairo Univ 2012;80:185-92.
- Kim E, Chotai S, Stonko D, et al. A retrospective review comparing two-year patient-reported outcomes, costs, and healthcare resource utilization for TLIF vs. PLF for single-level degenerative spondylolisthesis. Eur Spine J 2018;27:661-9. [Crossref] [PubMed]
- Kelly JP, Alcala-Marquez C, Dawson JM, et al. Treatment of degenerative spondylolisthesis by instrumented posterolateral versus instrumented posterolateral with transforaminal lumbar interbody single-level fusion. J Spine Surg 2019;5:351-7. [Crossref] [PubMed]
- Fujimori T, Le H, Schairer WW, et al. Does Transforaminal Lumbar Interbody Fusion Have Advantages over Posterolateral Lumbar Fusion for Degenerative Spondylolisthesis? Global Spine J 2015;5:102-9. [Crossref] [PubMed]
- Liu J, Deng H, Long X, et al. A comparative study of perioperative complications between transforaminal versus posterior lumbar interbody fusion in degenerative lumbar spondylolisthesis. Eur Spine J 2016;25:1575-80. [Crossref] [PubMed]
- Phan K, Rao PJ, Scherman DB, et al. Lateral lumbar interbody fusion for sagittal balance correction and spinal deformity. J Clin Neurosci 2015;22:1714-21. [Crossref] [PubMed]
- von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS Med 2007;4:e296. [Crossref] [PubMed]
- Abbasi H, Abbasi A. Oblique Lateral Lumbar Interbody Fusion (OLLIF): Technical Notes and Early Results of a Single Surgeon Comparative Study. Cureus 2015;7:e351. [Crossref] [PubMed]
- Allain J, Dufour T. Anterior lumbar fusion techniques: ALIF, OLIF, DLIF, LLIF, IXLIF. Orthop Traumatol Surg Res 2020;106:S149-57. [Crossref] [PubMed]
- Rabau O, Navarro-Ramirez R, Aziz M, et al. Lateral Lumbar Interbody Fusion (LLIF): An Update. Global Spine J 2020;10:17S-21S. [Crossref] [PubMed]
- Asher AL, Kerezoudis P, Mummaneni PV, et al. Defining the minimum clinically important difference for grade I degenerative lumbar spondylolisthesis: insights from the Quality Outcomes Database. Neurosurg Focus 2018;44:E2. [Crossref] [PubMed]
- Parker SL, Adogwa O, Paul AR, et al. Utility of minimum clinically important difference in assessing pain, disability, and health state after transforaminal lumbar interbody fusion for degenerative lumbar spondylolisthesis. J Neurosurg Spine 2011;14:598-604. [Crossref] [PubMed]
- Woodward J, Malone H, Witiw CD, et al. Transforaminal lumbar interbody fusion using a novel minimally invasive expandable interbody cage: patient-reported outcomes and radiographic parameters. J Neurosurg Spine 2021; Epub ahead of print. [Crossref]
- Hee HT, Castro FP Jr, Majd ME, et al. Anterior/posterior lumbar fusion versus transforaminal lumbar interbody fusion: analysis of complications and predictive factors. J Spinal Disord 2001;14:533-40. [Crossref] [PubMed]
- Potter BK, Freedman BA, Verwiebe EG, et al. Transforaminal lumbar interbody fusion: clinical and radiographic results and complications in 100 consecutive patients. J Spinal Disord Tech 2005;18:337-46. [Crossref] [PubMed]
- Schwender JD, Holly LT, Rouben DP, et al. Minimally invasive transforaminal lumbar interbody fusion (TLIF): technical feasibility and initial results. J Spinal Disord Tech 2005;18:S1-6. [Crossref] [PubMed]
- Patel AA, Zfass-Mendez M, Lebwohl NH, et al. Minimally Invasive Versus Open Lumbar Fusion: A Comparison of Blood Loss, Surgical Complications, and Hospital Course. Iowa Orthop J 2015;35:130-4.
- Vaidya R, Sethi A, Bartol S, et al. Complications in the use of rhBMP-2 in PEEK cages for interbody spinal fusions. J Spinal Disord Tech 2008;21:557-62. [Crossref] [PubMed]
- Christensen A, Høy K, Bünger C, et al. Transforaminal lumbar interbody fusion vs. posterolateral instrumented fusion: cost-utility evaluation along side an RCT with a 2-year follow-up. Eur Spine J 2014;23:1137-43. [Crossref] [PubMed]
- Rezk EMA, Elkholy AR, Shamhoot EA. Transforaminal lumbar interbody fusion (TLIF) versus posterior lumbar interbody fusion (PLIF) in the treatment of single-level lumbar spondylolisthesis. Egypt J Neurosurg 2019;34:26.
- Zhang D, Mao K, Qiang X. Comparing minimally invasive transforaminal lumbar interbody fusion and posterior lumbar interbody fusion for spondylolisthesis. A STROBE-compliant observational study. Medicine 2017;96:e8011. [Crossref] [PubMed]


